Our client suffered septic shock and nearly died two weeks after her baby was delivered by C-section. The client had a prolonged labor with ruptured membranes, but the OB/GYN didn’t give antibiotics prior to the C-section surgery. A few days after the C-section, our client was discharged from the hospital with a slight fever and red incision, but the doctor assured her there was nothing to worry about. A week after discharge from the hospital our client became ill, but the OB/GYN didn’t recognize a serious infection was brewing deep inside her. Instead, the doctor prescribed a general antibiotic for a red and oozing incision diagnosed as a “superficial wound infection.”
Before antibiotics were discovered, women with ruptured membranes and prolonged labor often died during childbirth. When a pregnant woman’s amniotic sac ruptures (“breaking water”), infection can occur because there is no longer any protective barrier between the outside of the mother’s body and the inside of the uterus where the placenta attaches, allowing bacteria to invade the uterine muscle tissue. This condition is called “endometritis,” but in the “old days” (before antibiotics were invented), this condition was known as “childbed fever.” Bacteria can also invade the amniotic sac and lining, known as “amnionitis” or “chorioamnionitis.” After antibiotics were invented, women rarely died from infection due to prolonged labor and ruptured membranes.
The standard of care for OB/GYN physicians requires prophylactic (preventative) antibiotics for women with prolonged labor and ruptured membranes, especially when a C-section is performed. When the patient’s abdomen and uterus are surgically opened, infected amniotic fluid can splash inside the abdomen, resulting in multiple “pus pockets” and serious widespread infection.
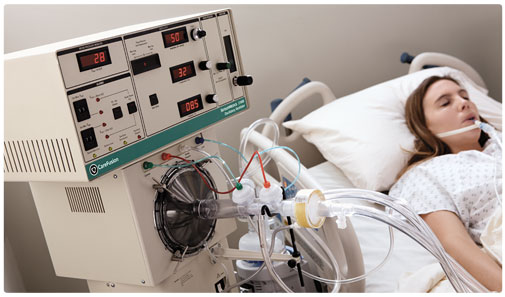
Approximately 2 weeks after the C-section our client suffered septic shock and nearly died. She underwent 7 surgeries to remove large “pus pockets” that had accumulated in her abdomen and spent nearly 2 months in the ICU. One of the surgeries included a colostomy because her bowels stopped working, which required a colostomy and collection bag for several months. Because of her extended illness and multiple surgeries, our client was unable to hold her baby for the first time until he was nearly one year old. When our client finally healed from all the surgeries, her abdomen was badly scarred and mutilated.
The defendant OB/GYN doctor alleged the standard of care did not require prophylactic antibiotics and that the patient’s septic shock was allegedly due to c. difficile colitis from the general antibiotic prescribed for the misdiagnosed “superficial wound infection” a week after the surgery.
We offered to settle our client’s case without trial for $1,250,000, but the defendant doctor and his insurance company refused to pay more than $50,000. After a 5-week trial, the jury agreed with our theory of the case and awarded $3,000,000 to our client.
*Ms. Chalfant’s jury verdicts and successful settlements do not guarantee the same or similar result for every case but are presented to demonstrate her knowledge of medicine, medical malpractice litigation skills, and successful track record. Every case is unique with varying facts and circumstances.